
THE DEEPER DIVE:
COGNITIVE BEHAVIORAL THERAPY FOR
PSYCHOSIS
FOR LICENSED PRACTITIONERS
Valerie Kreider, Ph.D.
BeST Center, Northeast Ohio Medical University
Harry Sivec, Ph.D.
BeST Center, Northeast Ohio Medical University
1
2
POLL #1
Experience Poll
Content
Group Activity
Orient client to treatment
Psychoeducation
Teaching CBT model
Stress Bucket
Stress Bucket Practice
Structure of Sessions
START Practice
Socratic Dialogue
Formulation
Take
-Home Work
Session 1: First Things First (First Section)
WHAT I HOPE YOU WILL TAKE WITH YOU TODAY
Structure of sessions
Orientation to and
initial psychoeducation
of client to the therapy
process
Working with Thoughts,
Emotions, and Behavior
The importance of
formulation-based
therapy
Guided Discovery
through Socratic
Questioning
Working through
Hallucinations,
Delusions, Negative
Symptoms
Summaries and
feedback
Adherence and
Special Topics
Taking Care of Yourself
44
COMPONENTS OF CBT-P
1. Engagement
2. Assessment
3. Recovery model thinking
4. Interventions
1. Positive symptoms
2. Negative symptoms
3. Distress
5. Treatment on a continuum
6. Integrated Team approach
7. Beginning, middle, and end of session
and of therapy
8. WRAP-ing it up – relapse prevention
55
AND SO THE TREATMENT BEGINS – CHECK OFF LIST
Adherence
Engagement
Psychoeducation
Guided Discovery
• Socratic Questioning
• Exploring voices
Delusions
Hallucinations
Cognitive Symptoms
Negative Symptoms
6
66
Relapse Prevention

PUT XAVIER AMADOR’S YOUTUBE VIDEO ABOUT LEAP HERE
(I’M NOT SICK, I DON’T NEED HELP. TEDXORIENTHARBOR, YOUTUBE)
7
77
I’m Not Sick!
I Don’t Need Help!
by Xavier Amador
330-325-6695 •neomed.edu/bestcenter • [email protected] • best schizophrenia practices

EXPECTATIONS OF THERAPY
That is, the client’s expectations of therapy.
• Clients may have been through treatment
or therapy that was shaming or at least
unhelpful
• Find out what was helpful and not so
helpful
• Ask if there are any things that might be
helpful in this therapy with you
Let them know that they can disagree with
you, be angry with you, ask questions, give
feedback, at any time
• They don’t need to wait to speak up
• You can hear anything they might need to
share
• Conversations are confidential unless of
threat of harm
10
1010
330-325-6695 •neomed.edu/bestcenter • bestcenter@neomed.edu • best schizophrenia practices
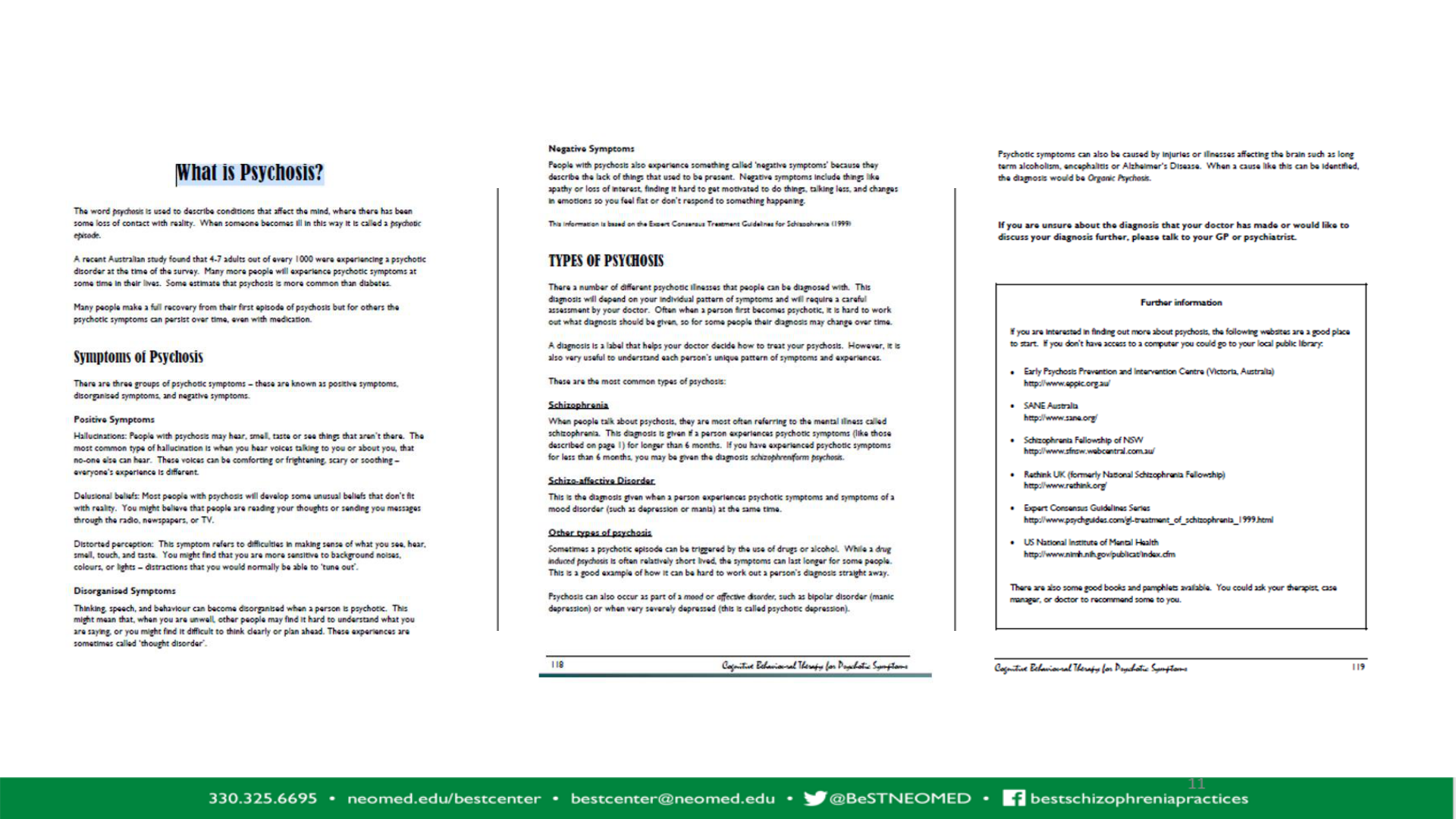
PSYCHOEDUCATION
• Give “What is Psychosis” handout
– (Page 6 of Day Two Handout Packet)
• Write the symptoms on a dry erase board
• Ask the client what he/she is experiencing that
looks like what is up on the board
• Review the handout with the client and discuss
• Ask for feedback, concerns, or questions
• You may choose to use more or less time talking
about the diagnosis depending on client’s
openness
11
1111
Voices that are nasty
People are following me
I’m sure I have worms
in my arms – I can
feel them wiggling
under my skin
Voices are telling me
that I’m not allowed
to eat
S2: p 6
S2: p. 6

WHERE ARE THE VOICES COMING FROM?
WHAT’S HAPPENING TO ME?
• Important to begin this discussion with finding out what the client
understands about the diagnosis
– Q: If you could describe this experience you are having to someone who
knows nothing about it, how would you describe your experience?
– Q: What does schizophrenia/psychosis mean to you?
– Q: What kind of symptoms do you think other people with schizophrenia
might have
13
1313
BEGINNING PRACTICE WITH THE CLIENT
• Ask the client to remember a time that was distressing
or difficult (not the worst one – a mild one)
• Draw columns on a paper or on a white board
• Help them work through that incident using:
– Situation
– Thoughts they had about themselves in the
situation
– Emotions they had about the situation and
– Behaviors – what did they do about it
• You may have to do this a little at a time, or over again
several times before the client can internalize the idea
• Remind them often of how to distinguish between each
component.
14
1414
Situation Thoughts Emotions Behavior
Heard I’m being Scared Called the
Voices followed police
Work- Some Used focus-
Sheet relief activity -
from crochet and
my tv
therapist
KINDS OF ISSUES WE WILL ADDRESS IN OUR THERAPY
• Mostly, that’s up to you!
– This time is for you to use as you wish
• This treatment is not about me
treating you…
– It’s about us working together to help you to be who you want to be
– Learn about and meet the goals you want to meet
– To create a lovely and meaningful life
15
1515

PROS AND CONS OF DECIDING TO CHANGE THROUGH THERAPY
16
1616
ORIENT CLIENT TO THE CBT TRIANGLE AND
GET A TIMELINE (PERSONAL HISTORY)
Situation
Do
Feel
Think
Decided to try treatment
20 yo
5 yo
10 yo
15 yo
Birth
23 yo
25 yo
17 yo
FIRST Episode
Went to school
– it was fun!
Parents
drinking &
drugging
I said I’d never
do it, but I
tried alcohol
Made it through a year of
college. I would have been
the first in the family to
finish
College didn’t
work, had to
move home
Moved to a
group home
30 yo
Living in independent living,
alone, no friends, scared, lost
17
1717
S2, pp. 4-5
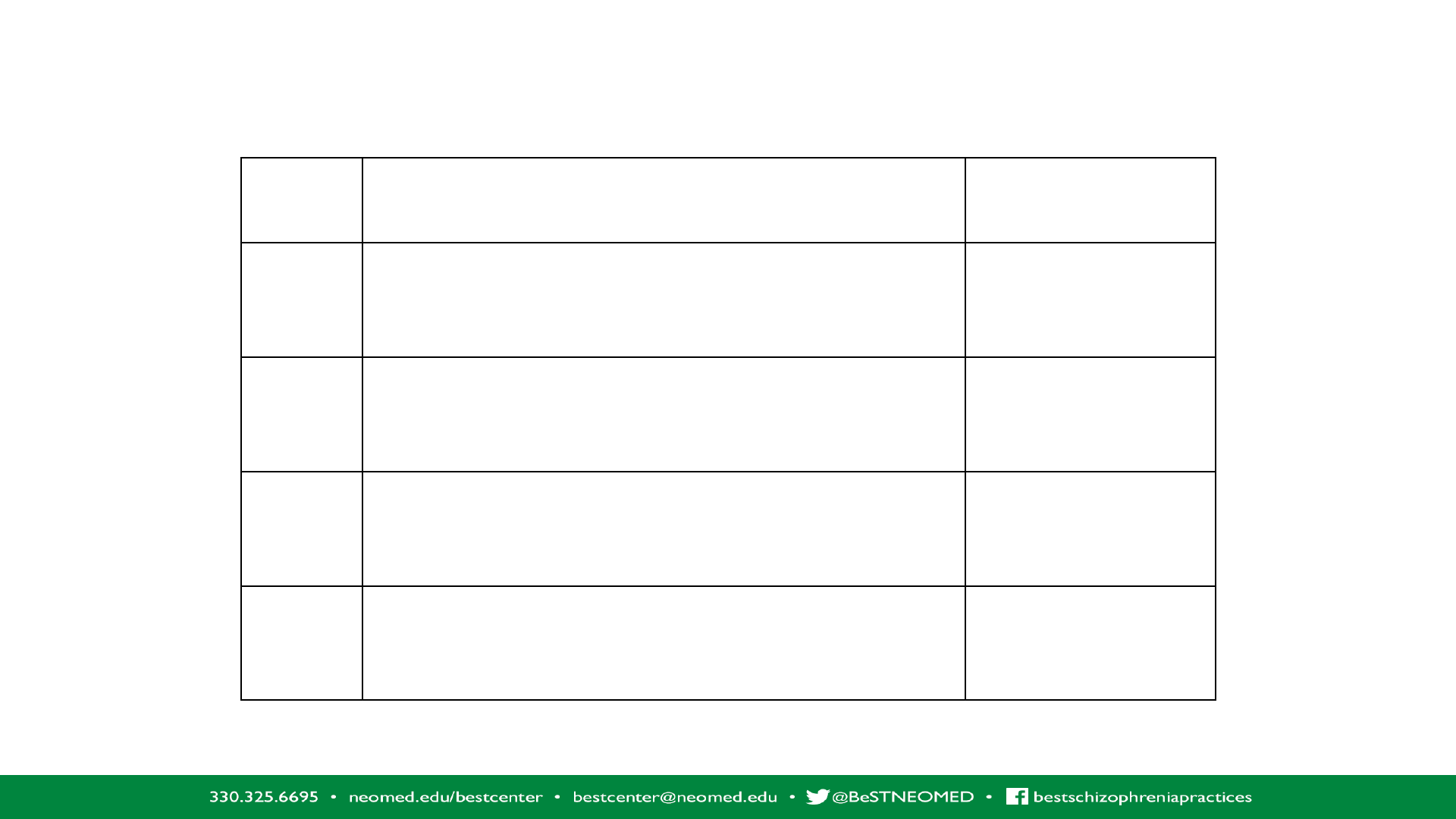
TIMELINE ACTIVITY
PAGE 5 IN DAY TWO HANDOUT PACKET
Age/Year
Experience
Health, Family, Education/Job, Significant Life Events, etc.
Meaning
What it meant to me at the time (e.g.
I was alone, unloved, unfairly treated,
others hurt me, rejected me…)
0 to 5
6 to 10
11 to 15
16 to 20
S 2: pp. 4-5
ASK THE CLIENT WHAT THEY HAVE ALREADY
TRIED TO GET SOME PEACE
• They may have tried ways of quieting the voices that have helped
– Listening to music
– Talking back to the voices
– Singing
– Distraction
– Etc.
• Many times the existing coping strategies
make things worse
– Drugs and alcohol
– Isolating
– Self harm
Reinforce healthy ways of
staying in balance
19
1919

WHAT IF ANOSOGNOSIA IS PRESENTING
• Then there’s really no use in educating about schizophrenia early on
• Ever seen someone use a louder voice when the person they’re talking to is blind?
• Stick to what the client wants in his or her life
• Give a little push once in a while to see if anything has changed
20
2020

TEACHING ABOUT STRESS IS IMPORTANT
• Now might be great time to bring up the “Stress Bucket”
• Use the Stress Bucket worksheet to discover what stressors and current coping
skills the client is currently using
• Emphasis and affirm the use of helpful and healthy coping skills
• Spend some extra time on the “vulnerabilities” section of the worksheet
─ Grief ─ Drug/Alcohol Use
─ Bereavement ─ Physical/Sexual Abuse
─ PTSD ─ Bullying
21
2121
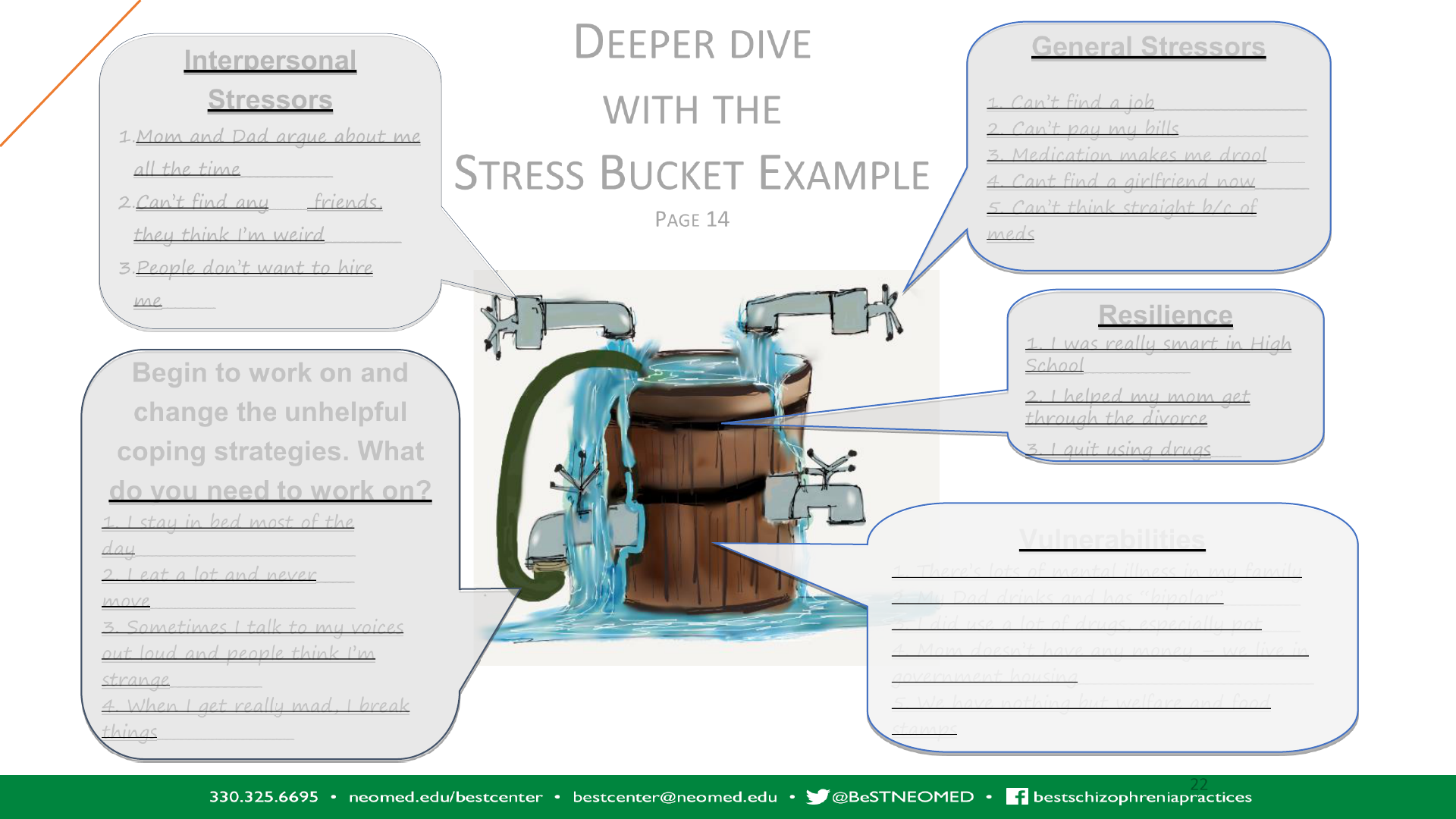
Interpersonal
Stressors
1.Mom and Dad argue about me
all the time____________
2.Can’t find any_____ friends,
they think I’m weird__________
3.People don’t want to hire
me_______
General Stressors
1. Can’t find a job____________________
2. Can’t pay my bills_________________
3. Medication makes me drool_____
4. Cant find a girlfriend now_______
5. Can’t think straight b/c of
meds
Resilience
1. I was really smart in High
School______________
2. I helped my mom get
through the divorce
3. I quit using drugs____
Vulnerabilities
1. There’s lots of mental illness in my family
2. My Dad drinks and has “bipolar”__________
3. I did use a lot of drugs, especially pot_____
4. Mom doesn’t have any money – we live in
government housing_______________________________
5. We have nothing but welfare and food
stamps
Begin to work on and
change the unhelpful
coping strategies. What
do you need to work on?
1. I stay in bed most of the
day_____________________________
2. I eat a lot and never_____
move___________________________
3. Sometimes I talk to my voices
out loud and people think I’m
strange____________
4. When I get really mad, I break
things__________________
DEEPER DIVE
WITH THE
STRESS BUCKET EXAMPLE
PAGE 14
2222
2222
Section 2: pp. 14-18
Looking at the Stress Bucket with your client
Collaboratively
Protective Factors
& Resilience
• Use of coping skills
• Social support
• Appropriate help seeking
• Regular use of medications
Risk Factors
&Vulnerabilities
• Drug and alcohol use
– Marijuana specifically
• Isolation
• Not happy with living space
• Living in critical atmosphere
• Write out each of these items (with brief explanation) on the worksheet
• Remember that the stress bucket can be used for present moment concerns, pasts
concerns, and future concerns
• It can also be used for a family session
232323

Interpersonal stress
= water going into
bucket
Family problems
Co-worker problems
Loneliness
General stressors
= water going into
bucket
Financial
Social
Work
Physical
Coping skills = thoughtful
release of stress through the use
of healthy coping skills
Reducing number of stressors
Non-judgmental stance
Acceptance
Listening
Responsive rather than reactive
Appropriate boundaries
Resilience = strength of
bucket’s wood and
bindings
Compassion
Patience
Empathy
Support
Effective communication
Spirituality
Family disruptions =
overflow of water
Arguments
Isolation
Chaos
Fighting
Vulnerabilities = size of bucket
Mental illness
Trauma
Substance abuse
Environment
(This includes family history of
all the above)
THE FAMILY FUSION STRESS BUCKET
242424

EFFECTIVE COPING STRATEGIES
• Ultimately, the goal is to keep too much water from getting
into the bucket
• Really work on finding effective coping strategies that the
client will really do
• This is a collaborative process
• This is also an excellent time to begin teaching relaxation
strategies for more immediate stress relief
25
2525
STRUCTURE OF SESSIONS
START
Section 2
2626
START STRUCTURE
Socializing:
~ 3” to 5”
•At the end of
socializing and
moving into the
Target zone, check
on homework
assigned from last
session (~5
to 10 minutes)
Target: ~ 2” to 10”
•Have client prioritize
the items to discuss
•Decide which item is
most important to
talk about today
•If you’ve picked
more than one topic,
and you didn’t get to
it, ask them if it’s ok
to address next time
(or should we make
time now?)
Action: ~ 15” to 25”
•Collaborate on what
might help with the
target issue using
CBTp techniques and
strategies If client is
having a hard time
with attention, have
them talk about their
issue in the last 10
minutes of the
session
Review: ~7” to 10”
•Have client review
the session
•Client to give
feedback to therapist
= 50-minute session
27
2727
Setting the agenda
START DEMO AND PRACTICE
TARGET: ORIENTING CLIENT
USING THE START STRUCTURE
2828
DEALING WITH DISORGANIZED THINKING
GUIDED DISCOVERY THROUGH SOCRATIC DIALOGUE
Section 3:
What is it and how do we use it in therapy
330-325-6695 •neomed.edu/bestcenter • [email protected] • bestschizophreniapracices
2929

A QUICK NOTE ABOUT GUIDED DISCOVERY &
SOCRATIC DIALOGUE
Helps to put some distance between the thought and the person
Helps the client arrive at his/her own conclusion
Means that you need to avoid giving the answers (WE DON’T HAVE THE ANSWERS)
Allows the client to be able to own their own answers and insight
Heightens awareness of the thoughts that leads to beliefs
Draws attention toward information the client has, though it is out of client’s focus
Builds self trust!
30
3030

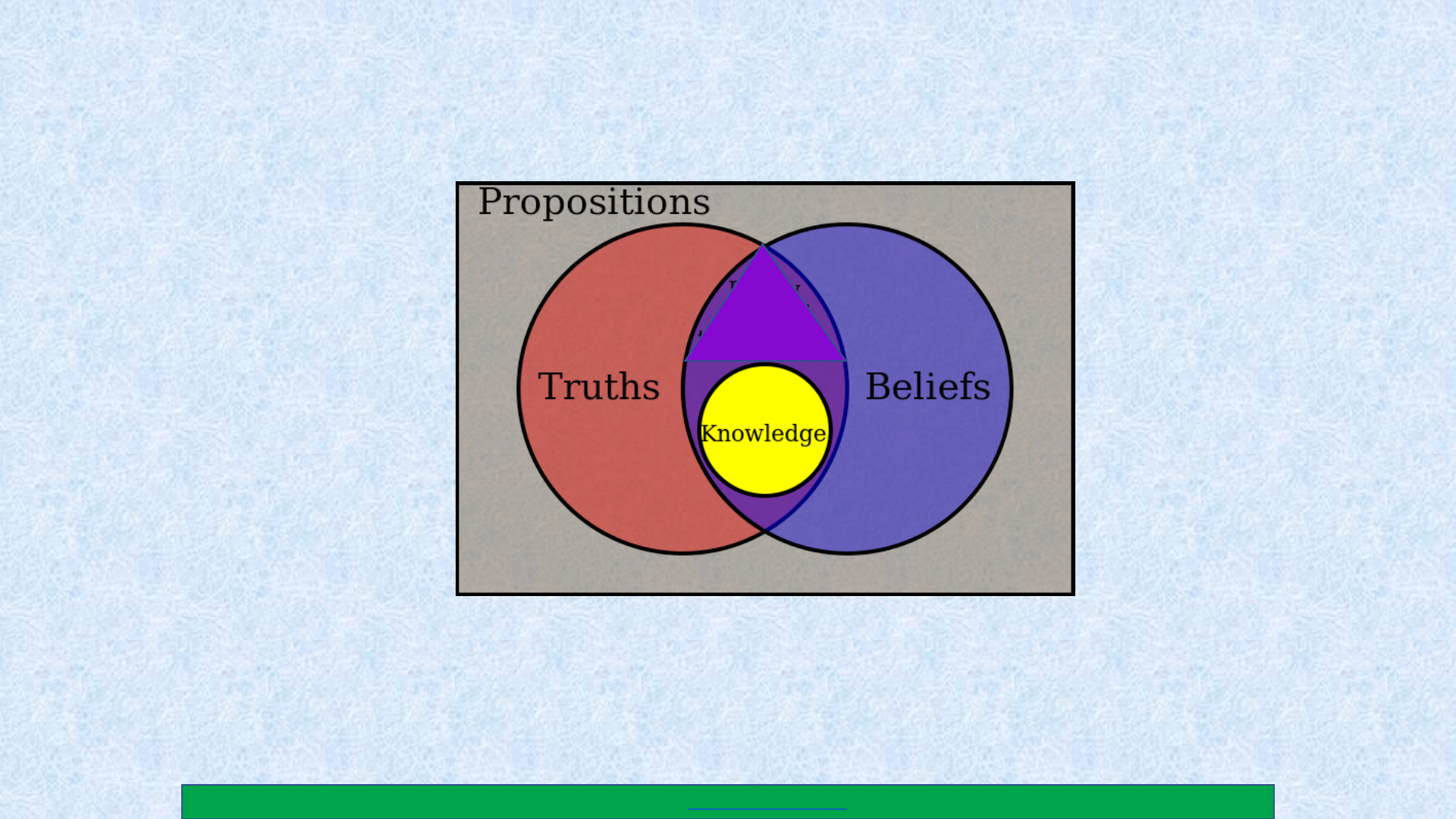
SOCRATIC DIALOGUE MINDSET
It is important to remember that when we engage in guided
discovery through Socratic Dialogue, we do it without knowing
the answer first
Guiding the client to a new way of thinking means we guide
them to a new way of thinking about their own thinking.
The client will often find a creative way to test his or her own
hypothesis with only minimal guidance from us
We can highlight the many routes one can take to discover a
solution, and we can teach that discovery process, but we
cannot find other people’s solution.
31
3131

GUIDED DISCOVERY
P. 10-13
• Guided discovery involves COLLABORATIVE EMPIRICISM
• Collaborative empiricism means that the client and therapist decide
TOGETHER how to evaluate a problem (voices, hallucinations, delusions),
and how to find solutions
• Our goal is to teach the client how to evaluate their own thoughts,
emotions, and behaviors so they can do it for themselves, for the rest of
their lives, on their own
32
3232
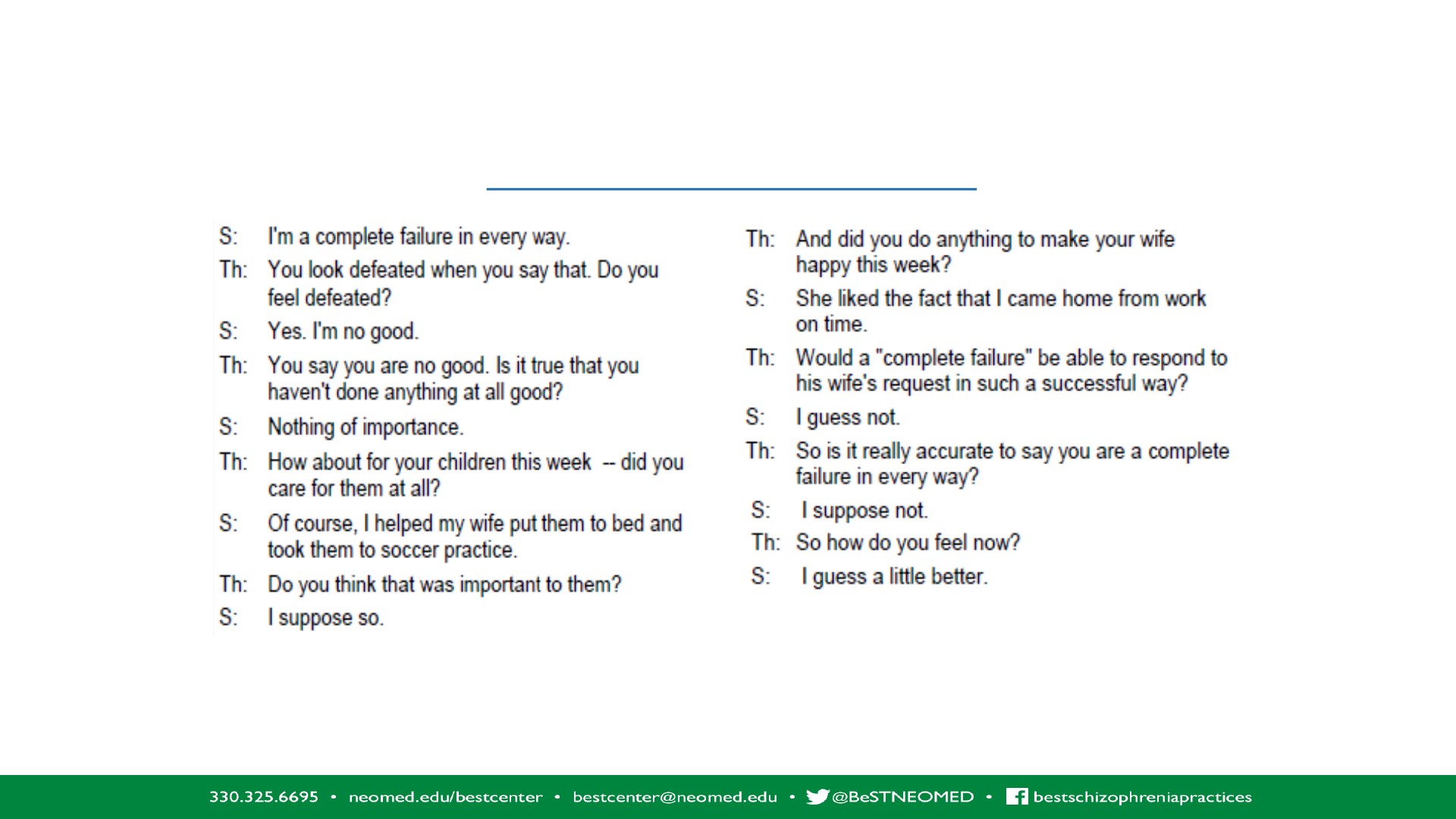
WHAT IS THE DIFFERENCE BETWEEN THE EXAMPLE SHOWN ON THIS SLIDE AND THE EXAMPLE
SHOWN ON THE NEXT SLIDE?
Padesky, C. Keynote address delivered at the European Congress of Behavioural and Cognitive Therapies, London, September 24, 1993
This article is included in the handouts that you received today, separate from the handout packet for day two
STUART AND HIS THERAPIST EXAMPLE 1
33
3333
S2: pp 10-13

STUART AND HIS THERAPIST EXAMPLE 2
Padesky, C. Keynote address delivered at the European Congress of Behavioural and Cognitive Therapies, London, September 24, 1993
Follow along with
the handout titled
“Guided Discovery
Through the use of
Socratic
Questioning”
34
3434
WHAT NOT TO DO….AND WHAT TO DO…
Some research shows
that the better we are
at Socratic Dialogue
and Guided Discovery,
the worse the alliance
becomes
Unless there is huge
trust in you by the
client, trying to talk
them out of their
delusion through use
of evidence will sound
dismissive to the
client
Be genuinely curious
and thoughtful about
how you can learn
more about what their
thoughts are, and how
they impact emotions
and behavior
Be empathetic. And
then just drop seeds
of information to
wonder about
35
3535
• Would anyone like to see an example of
guided discovery in action?
• Would anyone like to demonstrate Socratic
Dialogue
GUIDED DISCOVERY TECHNIQUES
• Behavioral experiments • Voice diaries
• Thought diaries • Socratic dialogue
• Cognitive restructuring • And many more!
• Stress Bucket
There are many ways we
use guided discovery
It is the general term we
use that describes a
process of guiding the
client to a different way of
thinking in order to solve
their own problems and
situations
36
3636

FORMULATION
Section 4:
Case conceptualization at
onset of therapy
330-325-6695 •neomed.edu/bestcenter • [email protected] • bestschizophreniapracices
3737
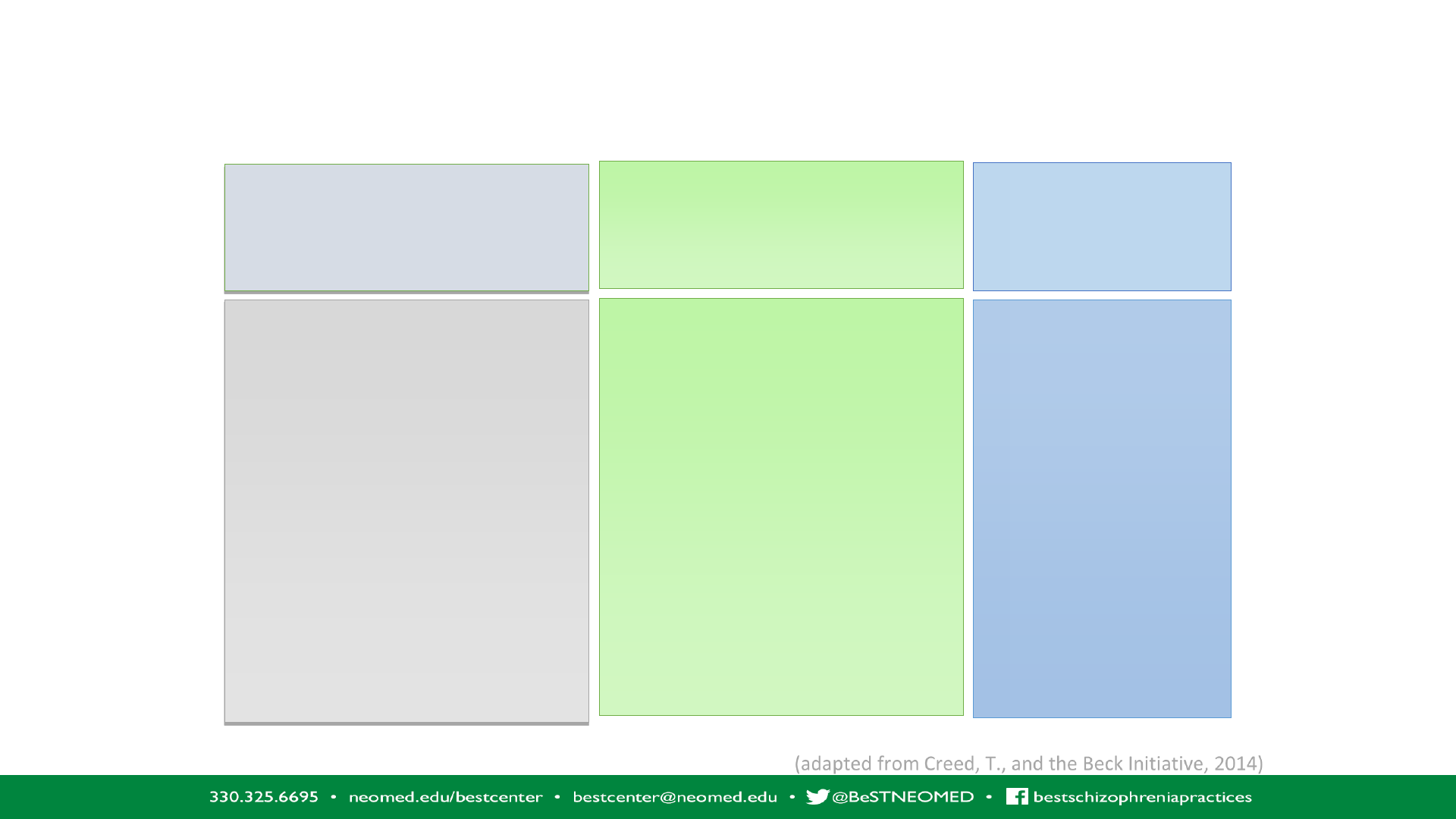
From Case Review to Formulation Based Thinking
Behavioral
target
History
Recent and Remote
Remember that always
behavior comes from
somewhere
What would it be like to be
this person – to walk in his
or her shoes?
Collaboration
on:
Behavior
Symptoms
Issues
That need to be
addressed
Thoughts lead to Beliefs
What is this person saying
to himself about the
problematic behavior,
situation, or distress?
What defeatist beliefs
might they hold about
themselves?
(adapted from Creed, T., and the Beck Initiative, 2014)
Thoughts/Beliefs
383838
WHAT IS A FORMULATION
Organizing information gathered from intake and assessment
Connect previous life history to current life issues and symptomology
What may have triggered the initial onset of symptoms
Discover what keeps the symptomology ongoing and distressing
What the client has already tried to reduce distress
What might stop the maintenance of distressing symptoms
A way to collaborate and build an alliance
Structures potential interventions
39
3939
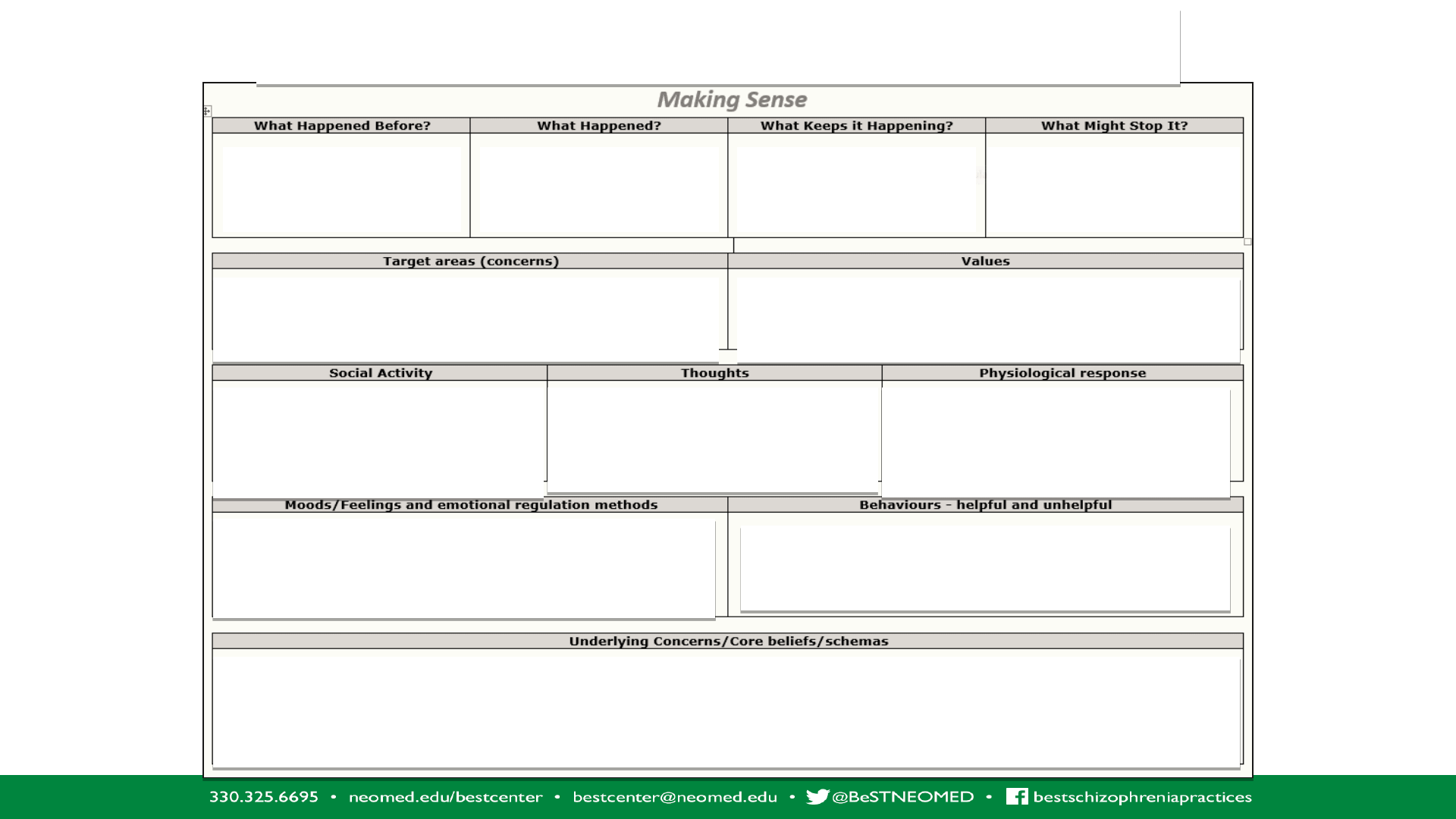
CASE FORMULATION
Predisposing
factors
Protective factors
Client and MHP need to agree on this
together
Client’s values –
not our values
What is the client saying to
him/herself about him/herself
in relation to the situation
Panic (list symptoms);
Depression (list symptoms);
Hallucinations (list)
Groups, clubs, hobbies,
even shopping can be
social
Be sure to check out your interpretation of
client’s mood/feelings; be sure to list helpful as
well as unhelpful ER methods client uses
Be sure to list helpful and unhelpful
behaviors
Once this section is completed, go over it with your client to make sure you’ve
got it right.
Precipitating
factors
Perpetuating
factors
404040
Handout S2:
pp 21, 22
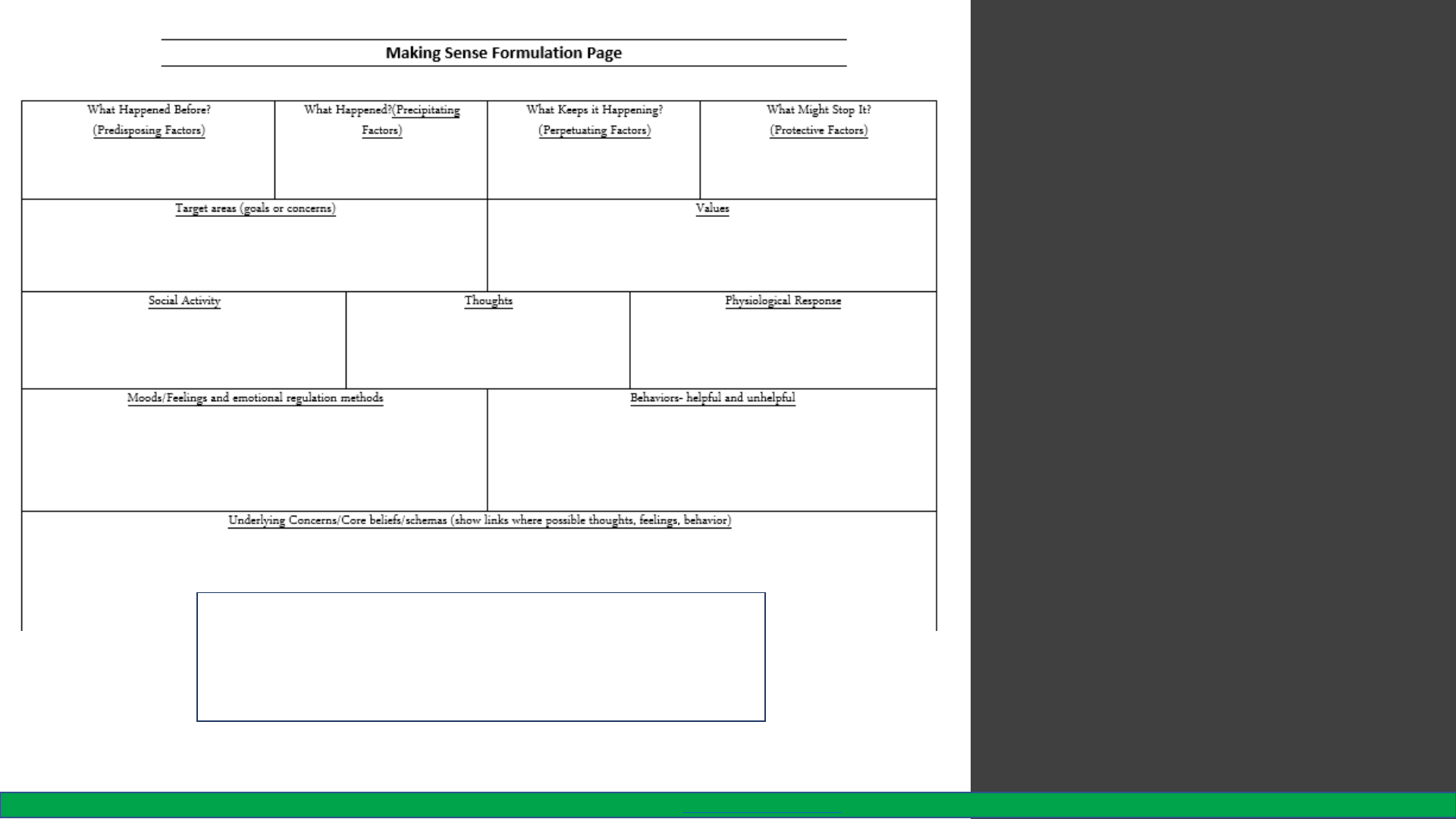
Case
Formulation
• It’s probably a good idea to
complete one of these as an
overall formulation for the client
• Fill out one briefly after an
appointment to get a better
understanding of what the client
is struggling with
• Return to that formulation with
the client to see if you have it
right. Adjust as needed.
• Use this as a guide for deciding
on interventions, treatment
planning, discharge planning, or
even as a monitoring tool.
414141
The “Making Sense” formulation sheet needs to be
handed in with each recording. No need to be
elaborate! “Brevity is the soul of wit”, (Shakespeare,
W., 1600, Hamlet)
330-325-6695 •neomed.edu/bestcenter • [email protected] • best schizophrenia practices

Case Formulation
List of common maintenance processes: This is how the client resists change
•Safety behaviors and avoidance
•Reduction of activity – withdrawal or isolation
•Catastrophic misinterpretations
•Self-fulling prophecies
•Performance anxiety
•Fear of Fear
•Perfectionism
•Short-term rewards
•Fear of consequences from voices
Tully, L.M. PowerPoint presentation. UCDavis https://behavioralhealth.ucdavis.edu/sites/g/files/dgvnsk2356/files/events/slides-
symposium/slides-psychosis-12-13-17/tully-121317.pdf
424242

POLLS 2 & 3

LET’S PRACTICE FORMULATION
We can help you to formulate several cases
Who’d like to begin?
4444

